Abstract
INTRODUCTION: Compared to pediatric population, treatment outcomes of adult B- lymphoblastic leukemia (B-ALL) remains dismal with long term disease free survival (DFS) of 40-45%. A high-risk subgroup of ALL called Ph-like ALL was recently identified based on similar genomic expression profile to Ph+ ALL, but with lack of Philadelphia (Ph+) chromosome. These patients have a variety of gene mutations/rearrangement including CRLF2, JAK2, KRAS, NRAS, PTPN11, ABL1, ABL2, CSF1R, PDGFRB, and they were shown to have high risk of disease relapse with poor survival outcomes. Although rare, certain Ph-like ALL patients have concurrent Ph+ chromosome and its clinical significance in Ph-like patients is largely unknown. The goal of our study was to characterize the prognostic impact of concurrent Ph+ chromosome on survival outcomes in Ph-like B-ALL patients.
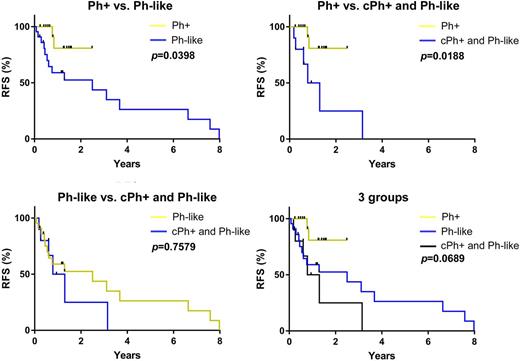
METHODS: Using Total Cancer Care (TCC) Moffitt Cancer Center (MCC) databases, we retrospectively identified B-ALL patients who had next generation sequencing (NGS) assessment (Foundation One®) from 2011 to 2017. BCR/ABL1 gene rearrangement was also assessed by fluorescence in-situ hybridization (FISH) or/and Quantitative RT-PCR. Clinical variables and disease-related prognostic factors were characterized at the time of diagnosis and annotated using descriptive statistics. The relapse free survival (RFS) and overall survival (OS) were estimated with the Kaplan-Meier method and compared using log-rank test. All statistical analyses were performed using SPSS v24.0.
RESULTS: A total of 50 B-ALL patients were included in this study. The median age was 49 (21-80) years and male patients were 66% (n=33). A total of 34% (n=17) patients had Ph+ only, 46% (n=23) patients had Ph-like mutations/rearrangement only, and 20% (n=10) patients had concomitant Ph+ and Ph-like features (cPh+ and Ph-like) based on NGS assessments. MLL / KMT2A gene rearrangement was identified in 10% (n=5) patients, and 43% patients had positive BCR-ABL1 transcript (p190, n=21; p210, n=3; p190/p210, n=3). In Ph-like patients, the most common mutation/rearrangement was IKZF1 (n=8) followed by IGH-CRLF2 rearrangement (n=7), KRAS (n=7), JAK2 (n=5), NRAS (n=4), FLT3 (n=3), PTPN11 (n=2) mutations and P2RY8-CRLF2 (n=1) rearrangement. The median number of Ph-like changes was 1 (0-4). A total of 82% (14/17) Ph+ patients were treated with TKI (imatinib, n=1; dasatinib, n=13) and 30% (3/10) of patients with cPh+ and Ph-like were treated with dasatinib in their induction chemotherapy. Allogeneic stem cell transplant was given to 15 patients. The median follow-up was 13.8 months (2-165). Median RFS in Ph+ patients was significantly longer than patients with Ph-like (NR vs. 11.6 months, p=0.0398) or cPh+ and Ph-like (NR vs. 7.4 months, p=0.0188), but there was no median RFS difference between Ph-like vs. cPh+ and Ph-like (11.6 vs. 7.4 months, p=0.7579), suggesting that cPh+ in Ph-like patients may not confer additional adverse impact on RFS. Median OS was not statistically different between three groups (NR in all groups, p=0.1486).
CONCLUSIONS: In B-ALL patients, Ph+ only patients had superior RFS compared to Ph-like patients regardless of the presence or absence of concurrent Ph gene rearrangement. Also, cPh+ in Ph-like patients was not associated with inferior RFS compared to Ph-like alone although the transcript levels of Ph gene rearrangement were low in most of the cPh+ cases. These results warrant further study regarding the prognostic impact of TKI in Ph-like patients with higher expression level of concurrent Ph gene rearrangement.
Lancet: Bio-Path Holdings: Consultancy; BioSight: Consultancy; Pfizer: Other: Institutional research funding, Research Funding; Janssen: Consultancy; Jazz Pharmaceuticals: Consultancy; Boehringer Ingelheim: Consultancy; Celgene: Consultancy; Erytech: Consultancy; Novartis: Consultancy. Chavez: Incyte: Membership on an entity's Board of Directors or advisory committees; Abbvie: Speakers Bureau; Janssen: Speakers Bureau; Kite: Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal